What is Mpox?
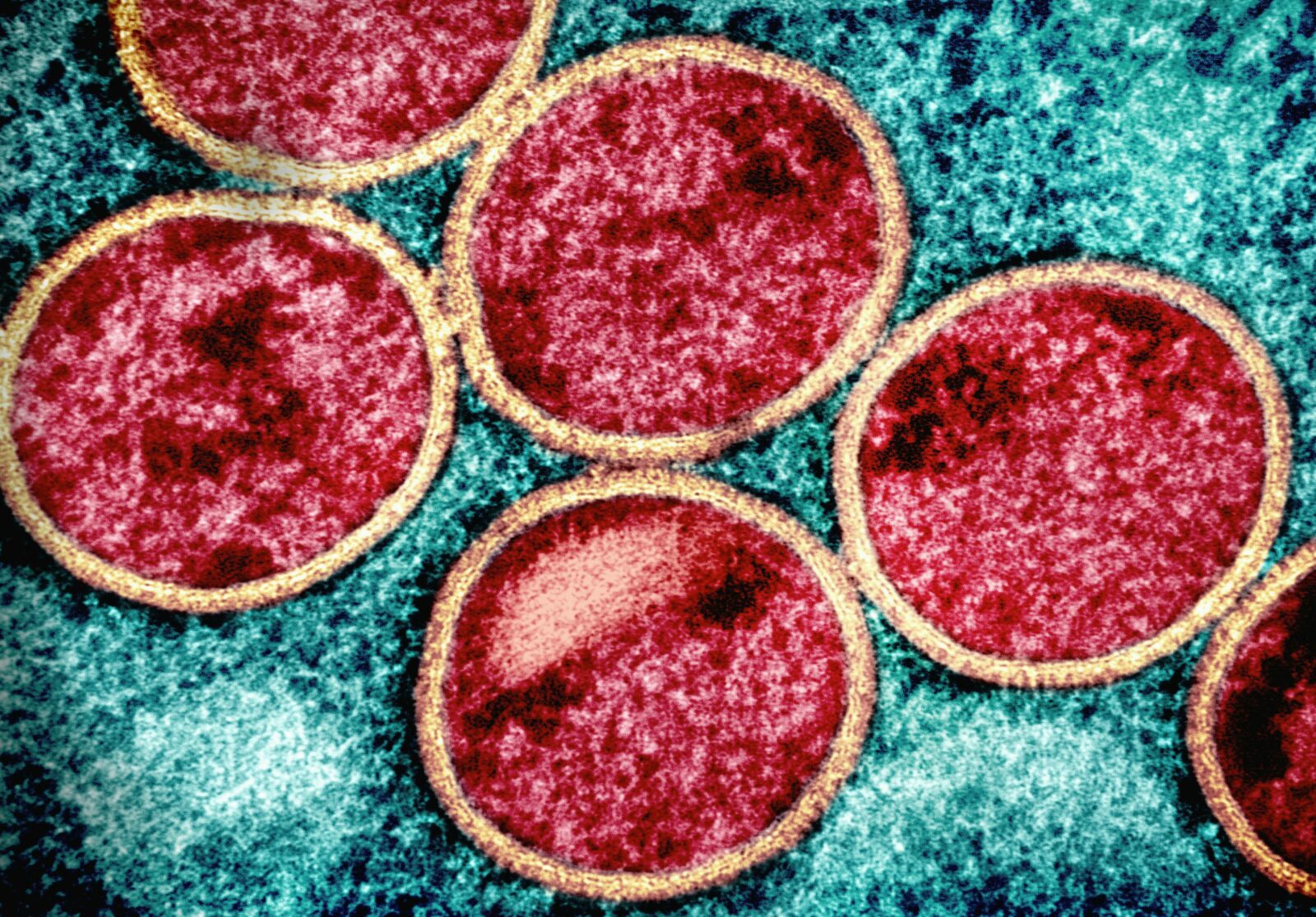
Mpox, formerly known as Monkeypox, was previously considered to be a rare but serious communicable and zoonotic disease that is caused by the monkeypox virus (MPXV), and a member of the orthopoxvirus genus and close relative of the variola virus which is responsible for smallpox. The name monkeypox, which has been changed to mpox, got its origin from the discovery of the virus in 1958, during an outbreak among monkeys in a Danish Laboratory.
To clarify, communicable, or infectious diseases, are caused by microorganisms such as bacteria, viruses, parasites and fungi that can be spread, directly or indirectly, from one person to another. Some are transmitted through bites from insects while others are caused by ingesting contaminated food or water.
Whilst a zoonotic disease is an infectious disease that has jumped from a non-human animal to humans. Zoonotic pathogens may be bacterial, viral or parasitic, or may involve unconventional agents and can spread to humans through direct contact or through food, water or the environment.
What’s the history?
Human Monkeypox was first identified in humans in 1970 in the Democratic Republic of the Congo in a 9-month-old boy in a region where smallpox had been eliminated in 1968. Since then, most cases have been reported from rural, rainforest regions of the Congo Basin, particularly in the Democratic Republic of the Congo and human cases have increasingly been reported from across central and west Africa.
Since 1970, there have been several outbreaks of clusters of cases on the African Continent and beyond including in 1970 – 2018 in the DRC, 2003 in the USA, 2018 – 2021 in the UK, Israel and Singapore, and in 2022 in the UK, USA, Canada, France, Germany, Belgium, Spain, Portugal, Italy, Sweden and Australia.
What’s happening with the current outbreak?
Unfortunately, the worry is legit when it comes to this not so fresh infectious disease which is making a serious and explosive comeback in endemic or typical locations and alarmingly also expanding its debut in non endemic or new countries and regions, including for the first time in Guyana, the confirmation of two cases of Mpox in 2022 during that outbreak.
Now in 2024, although cases were being reported in “endemic” African countries, the latest and significant upsurge in cases within the African continent and beyond resulted in the declaration of a Public Health Emergency of International Concern (PHEIC), from the World Health Organization (WHO) on August 14, 2024, the world’s premier authority on all health-related matters.
A PHEIC declaration is a serious matter reserved for the most worrying infectious disease outbreaks, it is the highest level of declaration from the WHO, which alerts the world to take substantial steps to protect their populations by scaling up public health resources to prevent, detect, diagnose, manage and curtail the transmission of this disease. The most recent and memorable event that warranted a PHEIC declaration was the COVID-19 pandemic.
How is Mpox transmitted?
The Mpox virus can be transmitted by direct and / or indirect contact with infected persons, animals, and/or contaminated fomites (contaminated objects). Transmission includes vertical transmission from a pregnant mother to her unborn foetus, percutaneous inoculation (penetration of skin caused by syringes, needles, abrasions, etc.) and respiratory secretions. Once infected with the virus, it takes about 1 to 3 weeks for the signs and symptoms of the disease to appear.
What are the signs and symptoms?
Mpox has traditionally caused a general illness that includes fevers, chills, sore throat and muscle aches, with a characteristic rash that is important to differentiate from that of other diseases that cause a rash (e.g., varicella, smallpox). More recently, during the 2022 to 2023 multi-country outbreak, some patients presented with genital, anal, and/or oral lesions without the general illness. Systemic symptoms are common and may occur before the rash appears or shortly after.
What’s the skin rash like?
The skin rash may occur a few days before or a few days after the general signs and symptoms like fevers, chills, sore throat and muscle aches. The skin rash is typically a series of boils, sores and bumps that appear on the skin.
The mpox rash often begins on the face and spreads over the body, extending to the palms of the hands and soles of the feet. It can also start on other parts of the body where contact was made, such as the genitals. It starts as a flat sore, which develops into a blister filled with liquid that may be itchy or painful. As the rash heals, the lesions dry up, crust over and fall off.
Some people may have one or a few skin lesions and others have hundreds or more. These can appear anywhere on the body including palms of hands and soles of feet, face, mouth and throat, groin and genital areas, or the anus.
Some people also have painful swelling of their rectum (proctitis) or pain and difficulty when peeing (dysuria) or when swallowing.
People with mpox can pass the disease on to others until all sores have healed and a new layer of skin has formed. Some people can be infected without developing any symptoms. Although getting mpox from someone who is asymptomatic (not showing symptoms) has been reported, information is still limited on how common it is.
Children, pregnant people and people with weak immune systems, including people living with HIV that is not well controlled, are at higher risk for serious illness and death due to complications from mpox.
Some people with mpox become very sick. For example, the skin can become infected with bacteria, leading to abscesses or serious skin damage. Other complications include pneumonia; corneal infection with loss of vision; pain or difficulty swallowing; vomiting and diarrhoea causing dehydration or malnutrition; and infections of the blood (sepsis), brain (encephalitis), heart (myocarditis), rectum (proctitis), genital organs (balanitis) or urinary passages (urethritis). Mpox can be fatal in some cases.
How is it diagnosed?
It may be a bit difficult for a qualified healthcare professional to identify and diagnose Mpox by simple observation or via a physical examination, because other infections and conditions can look similar. Whilst the general signs and symptoms can present in almost all the different types of infectious diseases, the skin rash can look like other diseases that also cause a skin rash, such as, chickenpox, measles, bacterial skin infections, scabies, herpes, syphilis, other sexually transmitted infections, and medication-associated allergies.
The preferred laboratory test for mpox is detection of viral DNA by polymerase chain reaction (PCR). The best diagnostic specimens are taken directly from the rash – skin, fluid or crusts – collected by vigorous swabbing. In the absence of skin lesions, testing can be done using swabs of the throat or anus. Testing blood is not recommended. Antibody detection methods may not be useful as they do not distinguish between different orthopoxviruses.
In Guyana, healthcare professionals will take a specimen by swabbing the skin rash lesions, then sending the samples to the National Public Health Reference Laboratory (NPHRL), where PCR analysis is conducted, and results are reported between 12 to 24 hours.
Is there a need to be isolated?
Yes, due to the infectious nature of Mpox, suspected, probable and/or confirmed cases should be isolated or separated from others, immediately at home, in a controlled room or area with limited access to family members, healthcare personnel or the public. If lesions are present, the individual should be isolated until the lesions scab over, which takes about 2 to 4 weeks.
How is Mpox treated?
First and foremost, there isn’t a specific treatment or existing cure for Mpox, as it is super difficult to develop a cure for infectious diseases caused by virus. Therefore, the objective of treating a person with mpox is to take care of the rash, manage pain and prevent complications.
Treatment is principally symptomatic. Most immunocompetent patients with mpox have mild disease and will recover without medical intervention. However, some patients may require pain relief medication (e.g., for pain related to proctitis or tonsillitis). In addition, for conditions like proctitis, stool softeners, topical lidocaine, and/or sitz baths many need to be used. The use of antiviral therapy is controlled and restricted for select cases following specialist consultation. Secondary bacterial infections can occur in patients with mpox. Should a bacterial infection be suspected, the patient should receive appropriate antibiotic coverage; regimens should generally include agents that are used to treat soft tissue infections (e.g., those that cover both staphylococcal and streptococcal species).
Is there a Mpox vaccine?
Yes, there are vaccines available for use in humans which are approved by the WHO. Getting an mpox vaccine can help prevent infection (pre-exposure prophylaxis). It is recommended for people at high-risk of getting mpox, especially during an outbreak, such as health and care workers at risk of exposure; people in the same household or close community as someone who has mpox, including children; people who have multiple sex partners, including men who have sex with men; and sex workers of any gender and their clients. The vaccine can also be administered after a person has been in contact with someone who has mpox (post-exposure prophylaxis). In these cases, the vaccine should be given less than 4 days after contact with someone who has mpox. The vaccine can be given for up to 14 days if the person has not developed symptoms.
How to prevent Mpox?
Luckily, as with most infectious diseases there are a few simple things that can be done to prevent infection with Mpox. These include:
- Vaccination: High-risk groups and close contacts of positive cases should consult the Ministry of Health about vaccination.
- Stay Informed: Keep up with credible reports on Mpox in regions you might visit for work or vacation.
- Avoid Contact: Refrain from sexual or close skin-to-skin contact with people who have a rash resembling Mpox, especially in high-risk areas.
- Do not Share Items: Avoid touching or sharing objects and materials used by someone with Mpox.
- Hand Hygiene: Wash your hands frequently with soap and water, or use an alcohol-based hand sanitizer, especially before eating, touching your face, and after using the bathroom.
- Handwashing: It’s one of the best ways to protect yourself and others from getting sick.
In a nutshell: Mpox is a real deal concern. Lately, it’s clear that old and new diseases are making a comeback, thanks to booming populations, climate change, exploring new areas for mining, logging, farming, migration, and more global travel.
Stay woke with legit info, spread the knowledge, and keep it safe out there!