Introduction
Imagine a world where a mosquito bite could lead to debilitating health challenges. This is the reality of Lymphatic filariasis (LF), caused by thread-like parasitic worms such as Wuchereria bancrofti, Brugia malayi and Brugia timori. These worms damage the human lymphatic system, leading to sever conditions like lymphoedema, hydrocele and elephantiasis. In the Americas, W. bancrofti (Wb) is responsible for ninety percent of all cases of filariasis.
The disease is transmitted by various of mosquito vectors from the genera Anopheles, Aedes, Culex, Mansonia and Ochlerotatus. Its prevalence is particularly high in warm climates that support mosquito populations for extended intervals. For those affected, advanced stages can lead to profound stigma and social exclusion due to physical disfigurment.
In response to this public health challenge, the World Health Organization instituted the Global Programme to Eliminate Lymphatic Filariasis (GPELF) in the early 2000’s. This initiative aims to eliminate LF through targeted interventions designed to reduce its prevalence to a level where transmission is no longer sustainable. Two principal strategies include annual mass drug administration (MDA) for at-risk populations and comprehensive management of morbidity to prevent disability through the provision of the WHO recommended minimum package of care. The minimum package of care includes treating acute attacks, managing lymphedema, managing hydrocele and administering anti-filarial medicines.
In the Americas, approximately seventy percent (70%) of the population is considered at risk, with an estimated twelve million people at risk in three countries. including Guyana. Guyana being one of three countries with particularly high risk.
In Guyana, W. bancrofti is primarily transmitted by Culex mosquitoes, particularly Culex quinquefasciatus, which thrive in urban environments where human activity plays a significant role in their breeding. The transmission of W. bancrofti is relatively inefficient, necessitating numerous infectious bites to develop a detectable infection. Efforts to eliminate LF in Guyana have shown promising results, with significant reductions in disease prevalence across six (6) of the eight (8) endemic regions. To maintain the gains the Ministry of health recently concluded the first of two rounds of MDA using the triple drug therapy Ivermectin, Diethylcarbamzaine and Albendazole in regions three (3) and four (4) this year and the second round is to be implemented in 2025.
LF Transmission and Symptoms
When an infected mosquito takes a blood meal, it deposits a third stage larva onto the skin of a human host. These larvae then penetrate the skin and migrate to the lymphatic system, where they mature into adult worms over a period of six to twelve months. Once matured, the adult worms produce thousands of first stage sheathed larvae, known as microfilariae, for up to eight years.
When a female mosquito consumes a blood meal containing microfilariae, these larvae are ingested into its stomach. Within about twelve days, some of these microfilariae develop into infective third-stage larvae, which then migrate to the mosquito’s proboscis. The cycle continues when the mosquito feeds on another human host.
The risk of Lymphatic Filariasis infection correlates with the frequency and duration of exposure to infective mosquito bites, specifically the accumulation of adult worm antigens in the lymphatics. The presence of mature worms triggers an inflammatory response and can cause mechanical damage to the lymphatic tissues. Additionally, these worms exist in a symbiotic relationship with Wolbachia endobacteria, which are crucial for the growth and development of the filarial parasites and contribute to the inflammatory disease processes associated with infection.
The Spectrum of Symptoms
The impact of LF varies among individuals, affecting about one third of those infected. People living in endemic regions can be categorized into five groups.
- Uninfected but Exposed: Residents of at-risk areas who have not contracted the disease.
- Asymptomatic Infected: Individuals who carry the infection without symptoms but can transmit it.
- Acute Filariasis: People in this category experience sudden symptoms, such as fever and inflammation of the lymph nodes. Commonly affected areas include the groin and armpits, and men may face complications in their genital region. These acute episodes can cause significant discomfort and are often linked to immune responses to the dead or dying worms.
- Chronic Infection: Years after initial infection, individuals may develop chronic symptoms, such as swelling in the limbs, genitals, or breasts (lymphedema), and severe skin changes known as elephantiasis. These conditions arise from damage caused by adult worms, leading to blockages and infections.
- Tropical Pulmonary Eosinophilia (TPE): A syndrome marked by coughing, wheezing, weight loss, and fever, often occurring at night due to the behavior of the microfilariae.
- Other Health Issues: LF can also be linked to kidney problems and joint pain (monoarthritic).
Understanding these manifestations is crucial for addressing the health challenges posed by LF.
LF Treatment and Management
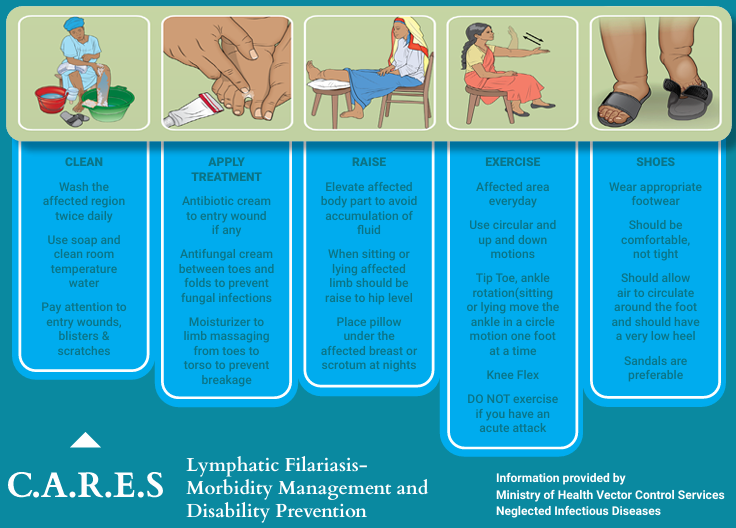
Effective management for LF both encompasses both preventative and pharmacological strategies. Patients are encouraged to maintain hygiene and care of the affected areas to prevent complications and reduce the severity of symptoms. The CARES method emphasizes Cleaning the affected limb, Applying topical treatments, Raising the limb to reduce fluid buildup, Exercising and wearing well-fitting Shoes.
Treatment includes anti-filarial medications administered through mass drug campaigns or clinically to target adult worms and microfilariae. Diethylcarbamazine (DEC) is the primary drug used, effective in killing adult worms noting that same is contraindicated in patients with onchocerciasis and in pregnant women. Ivermectin and albendazole help maintain lower microfilaria levels.
Doxycycline is effective against adult worms and improves lymphatic health when given over 4 to 8 weeks. For acute episodes, treatments typically include rest, limb elevation, and analgesics, with antibiotics prescribed for severe bacterial infections.
Ministry of Health’s Commitment to LF Elimination
The political will and commitment demonstrated by the Ministry of Health have positioned Guyana within the elimination continuum for Lymphatic Filariasis (LF), signifying that with consistent coordinated efforts by 2030 Guyana will eliminate this infectious disease from their shores. Following a remapping survey conducted in 2019, eight out of ten administrative regions were identified as endemic for LF. With support from the Pan American Health Organization and partners like USAID, the Ministry of Health successfully reduced the prevalence of LF in six of these regions-Regions 1, 2, 5, 6, 7, and 10. Regions 3 and 4 are the only areas still requiring mass drug administration (MDA), which is scheduled for two additional annual rounds in 2024 and 2025. MoH has also trained several clinicians, nurses and laboratory staff to adequately identify, treat and manage this preventable disease.
Your Role in the Fight Against LF
Communities in Guyana play a vital role in combatting (LF). Everyone aged two years, not pregnant nor seriously ill are encouraged to participate in MDA campaigns and take the Filaria pills alongside their families and friends. Residents should also their local health center for guidance on diagnostic and treatment options.
Additionally, communities can help by reducing mosquito breeding sites, such as eliminating standing water and improving sanitation.
Most importantly, citizens are encouraged to support those suffering from the chronic effects of LF. This includes seeking to understand how the disease is transmitted, recognizing its signs and symptoms, promoting the CARES approach, and offering kind words of support to combat the stigma and discrimination often associated with this illness. These efforts will ultimately contribute to improving public health and well-being in the community.
The Ministry of Health is dedicated to improving awareness of LF, increasing access to care and fostering open discussions to combat stigma and discrimination.
In conclusion, community engagement and education are crucial for the successful elimination of Lymphatic Filariasis in Guyana. By raising awareness, reducing stigma, and encouraging participation in health initiatives, we can work together to combat this disease, ultimately improving public health and the quality of life for all affected individuals.