Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder that affects about 10 percent of females. It can cause a variety of symptoms, including irregular periods, acne, excess facial or body hair, hair loss, and weight gain. While PCOS can be challenging to manage, understanding the condition and its treatments can help you take control of your health.
What Is PCOS?
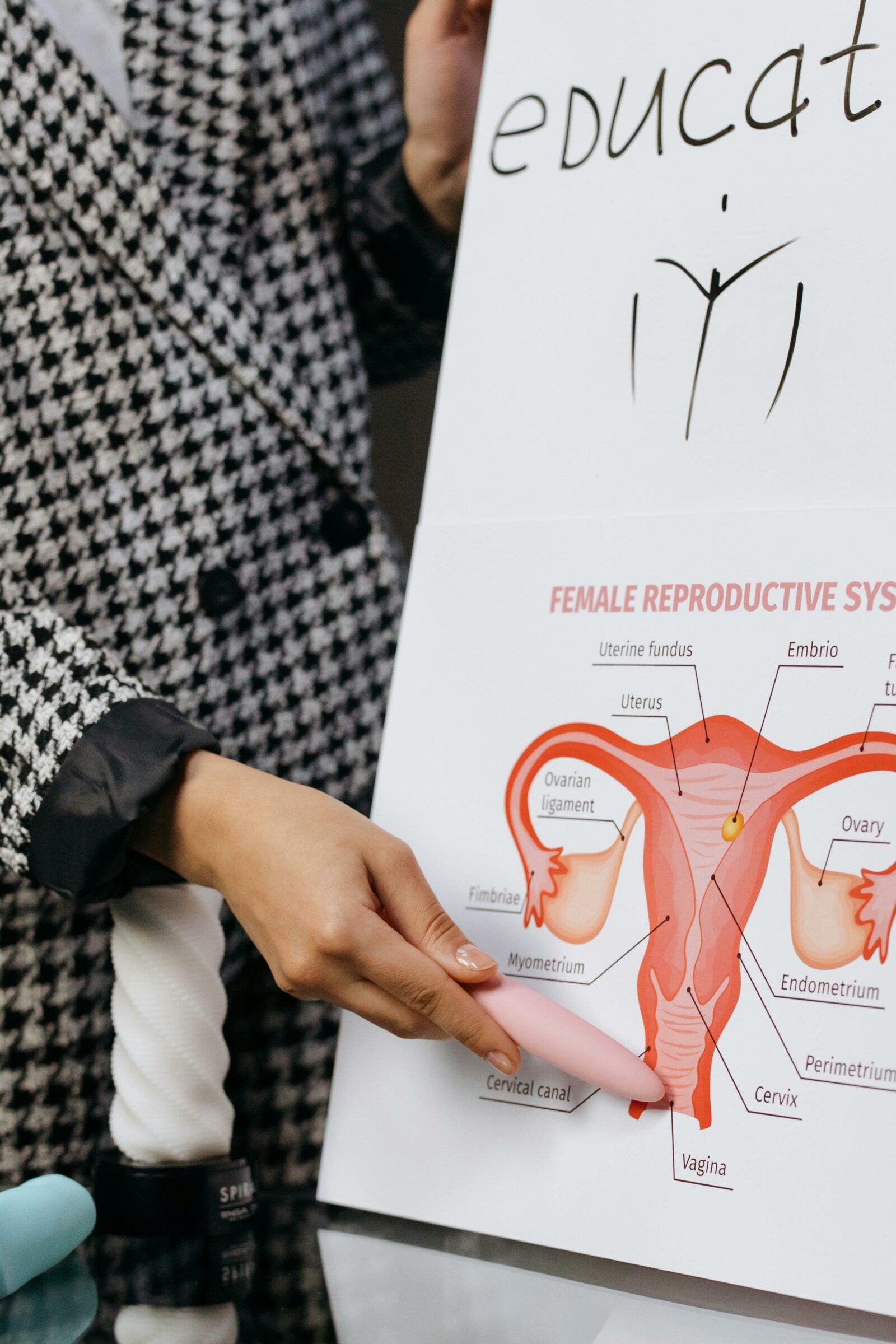
PCOS is a condition where the ovaries produce too many small follicles (tiny sacs that usually release eggs) instead of one mature follicle each month. This disrupts ovulation—the process where an egg is released—leading to irregular or missed periods. Additionally, the ovaries often produce higher-than-normal levels of testosterone, a hormone typically associated with males but present in all people. This hormonal imbalance causes many of the symptoms of PCOS.
What Causes PCOS?
The exact cause of PCOS is not fully understood, but several factors likely play a role:
- Insulin Resistance: Many people with PCOS have insulin resistance, meaning their bodies don’t use insulin effectively. This can lead to higher insulin levels, which may increase testosterone production.
- Hormonal Imbalance: Elevated testosterone and luteinizing hormone (LH) levels, along with low levels of sex hormone-binding globulin (SHBG), contribute to symptoms like excess hair growth and acne.
- Genetics: PCOS often runs in families, suggesting a genetic link.
Common Symptoms of PCOS
PCOS affects people differently, but common symptoms include:
- Irregular periods: Fewer than eight periods a year or very heavy periods.
- Excess hair growth (hirsutism): Thick, dark hair on the face, chest, or belly.
- Acne and oily skin: Often persistent and harder to treat.
- Hair thinning or loss: Typically, on the scalp.
- Weight gain or difficulty losing weight: Many with PCOS struggle with obesity.
- Fertility issues: Difficulty getting pregnant due to irregular ovulation.
Why Is It Important to See an OBGYN?
Even if your symptoms seem mild, seeing an OBGYN is crucial because PCOS increases the risk of other health problems, such as:
- Type 2 diabetes (due to insulin resistance).
- High cholesterol and heart disease.
- Sleep apnea (a condition where breathing stops briefly during sleep).
- Depression and anxiety.
- Eating disorders (like binge eating).
Early diagnosis and treatment can help manage symptoms and reduce these risks.
How Is PCOS Diagnosed?
There’s no single test for PCOS, but doctors typically use a combination of:
- Medical history and physical exam (checking for symptoms like excess hair or acne).
- Blood tests to measure hormone levels, blood sugar, and cholesterol.
- Pelvic ultrasound to look for multiple small follicles on the ovaries.
Your doctor may also rule out other conditions with similar symptoms, such as thyroid disorders.
Treatment Options for PCOS
While there’s no cure for PCOS, treatment can help manage symptoms and reduce long-term risks.
1. Birth Control Pills
- Regulate periods, reduce acne, and lower testosterone levels.
- Added benefit: Decrease the risk of uterine cancer (which is higher in people with irregular periods).
2. Anti-Androgen Medications
- Block testosterone effects, reducing acne and excess hair growth.
3. Progestogen Therapy
- Regulates periods and protects the uterus.
4. Metformin
- Improves insulin resistance, may help with weight loss, and can regulate periods.
5. Lifestyle Changes
Exercise: Regular physical activity helps with weight management and insulin sensitivity.
Weight management: Losing just 5% of your body weight (e.g., 10 pounds if you weigh 200 pounds) can improve symptoms.
Diet: Focus on whole foods, fiber, and low-glycemic-index carbs to manage insulin levels.
Supplements: work best alongside diet and exercise and can include: Inositol, Omega-3 Fatty Acids (EPA & DHA), Vitamin D, Magnesium, N-Acetylcysteine.

6. Fertility Treatments
If you’re trying to conceive, options include:
- Medical: Clomiphene or letrozole (to stimulate ovulation).
- Surgical: Ovarian drilling is a fertility-preserving, hormone-free option for patients struggling to ovulate, it offers a natural conception pathway for many.
- In vitro fertilization (IVF) in more severe cases.
7. Symptom-Specific Treatments
- Acne: Medicated creams or antibiotics.
- Excess hair: Laser therapy or electrolysis.
What will my life be like Living with PCOS?
PCOS is a lifelong condition, but with the right care, you can lead a healthy, full and normal life. Here are some tips:
- Stay consistent with treatments: Medications work best when taken as prescribed.
- Monitor your health: Regular check-ups for blood sugar, cholesterol, and blood pressure are important.
- Mental health matters: PCOS can affect self-esteem and mood. Don’t hesitate to seek support for anxiety or depression.
- Connect with others: Joining a PCOS support group can provide encouragement and shared experiences.
Recent Advances in PCOS Research
New studies continue to explore better treatments for PCOS, including:
- GLP-1 agonists (e.g., Ozempic, Mounjaro): Originally for diabetes, these drugs show promise in helping with weight loss which can be very difficult for these patients and insulin resistance in PCOS.
- Anti-inflammatory approaches: Since PCOS involves chronic low-grade inflammation, anti-inflammatory diets and supplements (like omega-3s) are being studied.
Final Thoughts
PCOS can be frustrating, but you’re not alone. With the right medical care, lifestyle adjustments, and support, you can manage symptoms and reduce long-term health risks. If you suspect you have PCOS or are struggling with symptoms, talk to your OBGYN—early intervention makes a big difference.
Remember, PCOS doesn’t define you. Many people with PCOS live full, active lives, and with the right tools, you can too.