Obesity
Obesity is defined as abnormal or excessive body fat accumulation that presents an increased risk for health problems. It is a multifactorial condition that contributes significantly to risk for many of the common non-communicable disease (NCDs) such as diabetes, cardiovascular diseases and cancers, that affect billions of people globally.
Body Mass Index or BMI calculation (weight in kilograms divided by height in meters squared) is the main screening tool used to assess whether an individual is obese (BMI of 30 or greater) or overweight (BMI between 25.0 and 29.9). Essentially, BMI describes the extent to which a person’s weight is appropriate for their height.
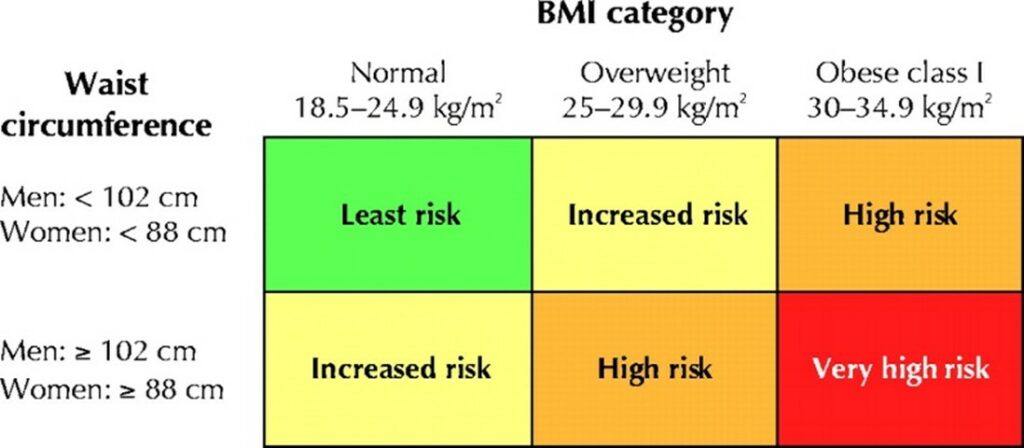
An increase BMI represents an overall increase in fat storage, locally (e.g. abdomen, buttocks, hips etc.) or distributed throughout the body. Waist circumference, which measures the amount of localized stored fat around the abdomen (belly) is also used by health professionals to provide complementary information about body fat and health risks, as shown in Figure 1. In both men and women progressive increase in either BMI or Waist Circumference is associated with high risk of health problems, However, when a person has both a high waist circumference and is also obese, the risk for health problems becomes very high.
Figure 1: Classification of obesity using BMI or Waist Circumference and risk for health problems
According to World Obesity Federation, the estimated prevalence of obesity in Guyana in 2025 is 20.2% among men; 35.5% women and 36.6% among children aged 5-19yrs. In 2016 the cost to healthcare associated with obesity in Guyana was $US Million 15.7; however, it is reasonable to expect that this has increased significantly as the number of people living with obesity progressively increases, along the concurrent increase in persons with NCDs needing more extensive and costly interventions.
Once viewed as a simple issue of overeating, obesity is now recognized as a complex interplay of genetics, lifestyle, environment, and metabolism. As such, understanding how obesity influences metabolic health is essential for clinicians, policymakers, and the public alike.
Metabolic Health
Metabolic health refers to the proper functioning of the body’s biochemical processes that regulate blood sugar, fats, blood pressure, and inflammation. A person is considered metabolically healthy when these factors are within a healthy range, regardless of body weight. However, excess body fat, particularly fat around abdomen and internal organs can disrupt these systems, leading to insulin resistance and diabetes, high blood sugar, high cholesterol levels, high blood pressure and chronic inflammation, among other health issues. Although the cause of obesity is multifactorial, some of the key causes include:
- Overeating
- High intake of processed, energy-dense foods, and excessive intakes of sugar and saturated fat, which are all characteristic of fast foods
- Lack of physical activity and sedentary lifestyles, which reduce energy expenditure
- Genetics and genes influence how we store fat, feel hunger, and burn calories
- Chronic stress and poor sleep disrupt cortisol and appetite-regulating hormones
The effect of poor dietary habits, particularly excessive calorie intake, on metabolic health is illustrated below in Figure 2.
Figure 2: The Metabolic Impact of Obesity
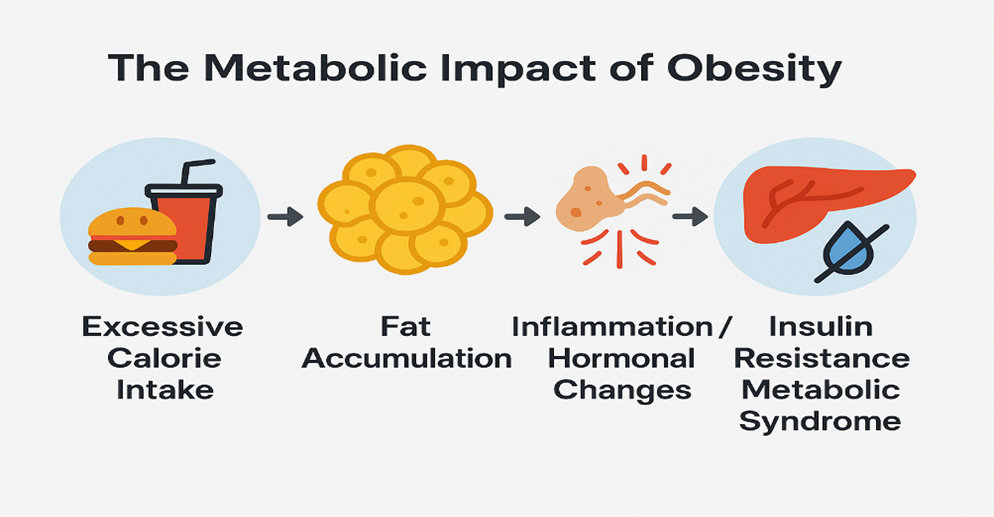
Much of the effects of obesity are largely due to how fat tissue behaves as it increases in our bodies. There is an increase in inflammation since enlarged fat cells secrete inflammatory metabolites that interfere with insulin signaling. Additionally, obesity impairs the normal function of the satiety hormones, leptin and adiponectin (anti-inflammatory), making it harder to regulate appetite and fat storage.
It is possible to successfully loose weight and improve metabolic health through dietary, lifestyle and pharmacological interventions. These approaches are best implemented under the guidance of a trained healthcare team that includes a nutritionist, lifestyle coach and physician experienced in weight loss management. Prevention and management strategies to promote weight loss include:
- Dietary approaches that emphasize whole, unprocessed foods: vegetables, fruits, whole grains, lean protein
- Reduce added sugars and refined carbohydrates, and
- Adoption of a healthy dietary pattern that emphasizes high consumption of plant-based foods including beans, lentils, fruits and vegetables (e.g. Mediterranean, DASH, Nordic or Portfolio diet).
Changes in dietary pattern must be accompanied by regular physical activity that includes a minimum of 150 minutes of moderate aerobic activity per week, and a bit of weightlifting to build muscle and improve insulin sensitivity. To support the changes in dietary and exercise behaviours it is important to get assistance or guidance from a friend or family of lifestyle coach to support these behavioral strategies. In particular, having a “buddy” to support adoption of these changes and associated anxiety, improves the success of weight loss programmes.
There are recently available many effective, evidence based pharmacological options that promote safe and effective, in the event that dietary and physical activity is not enough to promote weight loss, or if it is of benefit to achieve quick gradual weight loss. However, these must be supervised by an experienced physician. Over the past few years there have been a growth in the availability and use of semaglutides or appetite suppression drugs that promote effective weight loss; these are not approved for use in Guyana as yet, but their availability will most certainly make a difference to those who wish to lose weight. Although there are side effects with the use of these drugs, one of the beneficial effects, apart from weight loss, is the improvement of blood sugar control and in many cases a reversal of diabetes due to weight loss.
Public Health Implications
Obesity-related metabolic disorders are driving the rise in type 2 diabetes and cardiovascular disease, especially in lower-income and urban populations. As such a multi-level approach is needed: one that includes action such as clear warning labeling on foods containing high amounts of sugar, saturated fats and salt, nutrition education, improved access to fresh whole foods and implementation of early screening for metabolic risk in overweight patients.